Battery Ingestion Triage and Treatment Guideline
Battery Ingestion Triage and Treatment Guideline
©2010-2020 National Capital Poison Center. Reproduced and/or modified with permission.
Watch this video to learn more about the hazards of button batteries and steps towards prevention.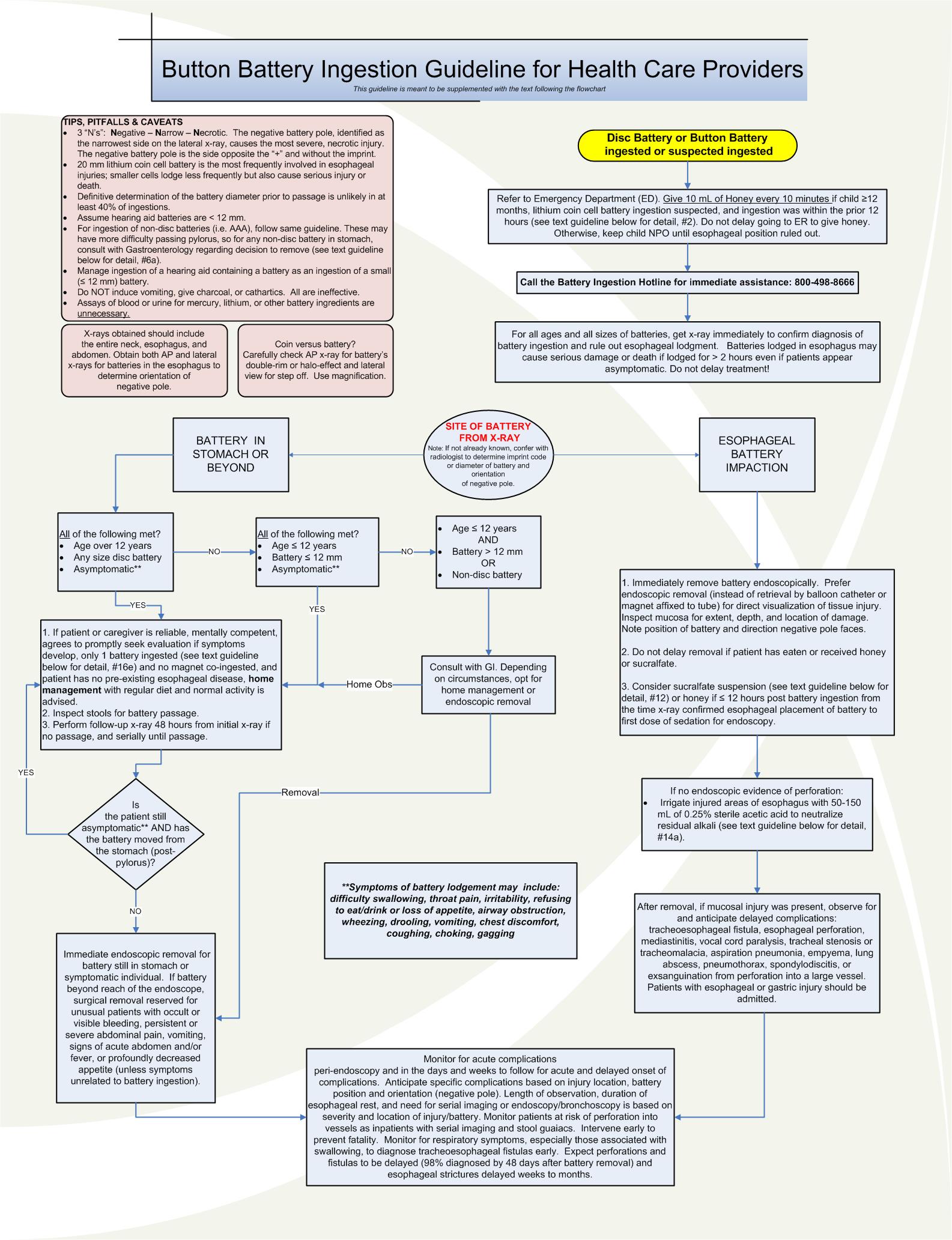
Battery Ingestion Triage and Treatment Guideline (text version)
Suspect the diagnosis:
Most serious battery ingestions are not witnessed. Consider the possibility of a battery ingestion in every patient with acute airway obstruction; wheezing or other noisy breathing; drooling; vomiting; chest pain or discomfort; abdominal pain; difficulty swallowing; decreased appetite or refusal to eat; or coughing, choking or gagging with eating or drinking. Suspect a button battery ingestion in every presumed “coin” or other foreign body ingestion. Carefully observe (zoom in on x-ray imaging) for the button battery’s double-rim or halo-effect on AP radiograph and step-off on the lateral view. Beware that the step-off may not be discernible if the battery is unusually thin or if the lateral film is not precisely perpendicular to the plane of the battery.
If battery ingestion is suspected:
- Do not induce vomiting.
- Administer honey immediately and while en route to the ER, if:
- A lithium coin cell may have been ingested (if you don’t know what kind of button battery was swallowed, assume it is a lithium coin cell unless it is a hearing aid battery);
- The child is 12 months of age or older (because honey is not safe in children younger than one year);
- The battery was swallowed within the prior 12 hours (because the risk that esophageal perforation is already present increases after 12 hours);
- The child is able to swallow; and
- Honey is immediately available.
How to dose honey:
a) Give 10 mL (2 teaspoons) of honey by mouth every 10 minutes for up to 6 doses. Do not worry about the exact dose or timing.
b) Use commercial honey if available, rather than specialized or artisanal honey (to avoid inadvertent use of large amounts of honey produced from potentially toxic flowers).
c) Honey is NOT a substitute for immediate removal of a battery lodged in the esophagus. Honey slows the development of battery injury but won’t stop it from occurring. Do not delay going to an ER to obtain or give honey.
Why give honey?
Honey is administered to coat the battery and prevent local generation of hydroxide, thereby delaying alkaline burns to adjacent tissue. Efficacy is based on a 2018 study (Anfang et al) assessing the in vitro protective effects of various liquids in the cadaveric porcine esophagus and in vivo protective effects of honey and sucralfate (Carafate®) compared to saline irrigations of batteries placed in the esophagus of live piglets. Both honey and sucralfate (Carafate®) effectively prevented the expected battery-induced pH increase and decreased the depth of the resulting esophageal injury.
- Other than giving honey, keep the patient NPO until an esophageal battery position is ruled out by x-ray.
- If the patient is asymptomatic, take up to 5 minutes to determine the imprint code from a companion or replacement battery, battery packaging, or product instructions. If no imprint code is available, measure or estimate the diameter based on the size of the slot the battery fits in or the size of a comparable battery. To estimate the battery diameter, compare the battery with a U.S. penny (19 mm) and nickel (21 mm). The radiologist can also assist with determining size (diameter), imprint of battery, and orientation of negative pole.
- Consult the National Battery Ingestion Hotline at 800-498-8666 for assistance in battery identification and patient management.
- Regardless of age of patient or size of battery, immediately obtain an x-ray to locate the battery. Batteries lodged in the esophagus may cause serious burns in as little as 2 hours. Do not wait for symptoms to develop. Patients with a battery in the esophagus may be asymptomatic initially. The 20 mm diameter lithium coin cell, with a diameter intermediate between a U.S. penny and nickel, is most frequently involved in esophageal injuries. Smaller cells lodge less frequently, but may also cause serious injury or death, especially in children younger than 1 year.
- Follow same guideline for ingestion of non-disc battery (ie AAA). While complications may be less since poles are farther apart, ingestion of cylindrical batteries may have more difficulty passing pylorus. For any non-disc battery in stomach, consult with Gastroenterology regarding decision to remove.
- If the patient is > 12 years, for any size battery and the patient is entirely asymptomatic and has been asymptomatic since the battery was ingested, home management with normal diet and activity can be done if these other criteria are met:
- Only one battery was ingested
- A magnet was not also ingested.
- There is no history of prior esophageal surgery, esophageal stricture/narrowing, motility disorders, or other esophageal disease.
- The patient (or caregiver) is reliable, mentally competent, and agrees to report symptoms that develop prior to battery passage, or over the subsequent month if passage is not documented, and understands the importance of promptly seeking evaluation for symptoms possibly related to the ingested battery.
- Stools can be inspected for battery passage.
- If battery not passed at 48 hours, another x-ray should be performed, and serially every 7-10 days thereafter.
- If the ingested battery is ≤ 12 mm and the patient is ≤ 12 and the patient is entirely asymptomatic and has been asymptomatic since the battery was ingested, home management with normal diet and activity can be done if these other criteria are met:
- Only one battery was ingested
- A magnet was not also ingested.
- The battery has been reliably identified based on imprint code or measurement of an identical cell, and the diameter is ≤ 12 mm. Definitive determination of the battery diameter prior to passage is unlikely in at least 40% of ingestions. Assume hearing aid batteries are less than 12 mm.
- There is no history of prior esophageal surgery, esophageal stricture/narrowing, motility disorders, or other esophageal disease.
- The patient (or caregiver) is reliable, mentally competent, and agrees to report symptoms that develop prior to battery passage, or over the subsequent month if passage is not documented, and understands the importance of promptly seeking evaluation for symptoms possibly related to the ingested battery.
- Stools can be inspected for battery passage.
- If battery not passed at 48 hours, repeat radiographs should be performed serially every 7-10 days thereafter until passage confirmed.
- If the patient is ≤ 12 years and the battery diameter is > 12 mm, gastroenterology consultation should be done. Depending on the status of the patient and/or other circumstances, the patient may undergo endoscopy for removal or be considered for home observation.
- X-rays obtained to locate the battery should include the entire neck, esophagus, and abdomen. Batteries located above the range of the x-ray have been missed, as have batteries assumed to be coins or cardiac monitor electrodes. On physical exam, check both ear canals and the nasal cavity to exclude battery insertion. Obtain both AP and lateral x-rays for batteries in the esophagus to determine orientation of the positive and negative poles. On the lateral film, the step-off is on the negative side of the battery. (The negative pole has a slightly smaller diameter, fitting within the battery can which forms the positive pole.) Anticipate complications based on battery position and orientation. Damage will be more severe in tissue adjacent to the negative pole.
- Immediately remove batteries lodged in the esophagus. Serious burns can occur in 2 hours.
- If possible, and if the child is able to swallow, administer sucralfate (Carafate® suspension, 1 g/10 mL). Give 10 mL PO every 10 minutes, up to 3 doses, from the time of x-ray determination that a battery is lodged in the esophagus until sedation is given for endoscopy. Honey has comparable efficacy (Anfang, 2018) and may be substituted for sucralfate suspension in children 12 months of age or older, dosed as outlined in #2, above. Do not give sucralfate or honey if the battery was possibly in the esophagus for more than 12 hours. Sucralfate or honey administration is not a substitute for emergent battery removal as these agents slow but do not eliminate tissue damage.
- Do not delay battery removal because a patient has eaten recently or because a patient was given honey or sucralfate (Carafate®) by mouth.
- Endoscopic removal is preferred as it allows direct visualization of tissue injury. After removal, inspect the mucosa surrounding the battery to determine the extent, depth, and location of tissue damage. Note the orientation of the battery in the esophagus: is the negative pole (side without the “+” and without the imprint) facing anteriorly or posteriorly? If possible, avoid pushing an esophageal battery into the stomach as the risk of esophageal perforation may increase.
- After a battery is removed from the esophagus, inspect the area endoscopically for evidence of perforation. If none is evident, irrigate the injured areas with 50 mL to 150 mL of 0.25% sterile acetic acid (obtained from the hospital pharmacy). Irrigate in increments and suction away excess fluid and debris through the endoscope. For decades toxicologists have advised against neutralization for fear of causing a thermal injury. However, a recent study (Jatana, 2016) using piglet esophagus preparations after button battery removal, showed only a minimal increase in temperature (0-3 °C), effective tissue surface pH neutralization, and decrease in the visible injury using this neutralization strategy. The tissue surface pH neutralization may reduce the development of progressive, delayed-onset esophageal injury after battery removal.
- After removing a battery from the esophagus, if mucosal injury was present, observe for delayed complications such as tracheoesophageal fistula, esophageal perforation, mediastinitis, vocal cord paralysis, tracheal stenosis or tracheomalacia, aspiration pneumonia, empyema, lung abscess, pneumothorax, spondylodiscitis, or exsanguination from perforation into a large vessel.
- Determine the length of observation, duration of esophageal rest, and need for serial imaging or endoscopy/bronchoscopy based on the severity and location of the injury, anticipating specific complications based on the injury location, battery position and orientation. Consider the proximity of the lodged battery and injured area to major arteries. Monitor patients at risk of fistulization into blood vessels carefully, as inpatients, with serial imaging (contrast CT or MRI of chest and/or neck) and stool guaiacs. Intervene early if perforation is imminent. Monitor for respiratory symptoms, especially with swallowing, to diagnose tracheoesophageal fistulas early.
- Expect delayed onset of esophageal perforations and fistulas involving the trachea or major vessels. Perforations were diagnosed by 48 days post removal in 98.1% of cases, and delays up to 27 days post removal were observed for esophageal-vascular fistulas. Recurrent laryngeal nerve injury may be evident on presentation or may not develop or be diagnosed for weeks after battery removal. Esophageal strictures and spondylodiscitis may not manifest for weeks to months post ingestion.
- Patients with esophageal injury should be admitted and observed due to the high risk of local edema developing with worsening symptoms, especially airway compromise when the battery is lodged high in the esophagus. In stable, well-appearing children, a clear liquid diet can be started after an esophagram shows no evidence of perforation. The esophagram is obtained at least 1-2 days after battery removal, earlier (1 day) for cases with mucosal injury only, and later for cases with deeper injury. Diet may be advanced to soft as tolerated, but all children who have had an esophageal battery removed should be limited to soft foods for a full 28 days to avoid mechanical damage to a healing esophagus. In children with more severe injuries, subsequent care and diagnostic intervention is guided by clinical manifestations.
- Patients with batteries removed from the upper esophagus should be monitored carefully for voice changes, respiratory distress, or stridor. If any of these are present or suggested, the cords should be visualized under direct laryngoscopic view in the awake patient to confirm bilateral vocal cord mobility. Unilateral or bilateral vocal cord paralysis is a common complication of battery ingestion due to damage to the recurrent laryngeal nerve(s). Paralysis may be delayed and not detected for days or weeks.
- Always consider the possibility of battery proximity to the aorta or other major vessels. If this is anatomically likely due to the position of the battery, use a contrast CT or MRI diagnostically to confirm there is at least 3 mm of tissue between the area of esophageal injury and adjacent vessels. Watch for sentinel bleeds, which may be subtle. Engage cardiothoracic surgery early if there is any possibility of an impending esophageal-vascular fistula.
- Retrieve batteries, endoscopically if possible, from the stomach or beyond if:
- A magnet was also ingested,
- The patient develops signs or symptoms that are likely related to the battery ingestion, or
- A button battery larger than a hearing aid battery (> 12 mm diameter), ingested by a child younger than or equal to 12 years, remains in the stomach for 48 hours or longer. Consult with Gastroenterologist in this setting as home observation may be possible depending on patient factors and/or circumstances. If battery diameter is unknown, estimate if from the x-ray, factoring out magnification (which tends to overestimate battery diameter).
- If a large button battery (≥ 20 mm) is in the stomach or beyond of a child younger than 5 years, and based on history, might have lodged in the esophagus for > 2 hours before passing to the stomach, consider diagnostic endoscopy to exclude the remote possibility of esophageal injury. (In a handful of cases, patients with significant and symptomatic esophageal injury have been found with batteries that have already passed beyond the esophagus.) If symptoms suggestive of esophageal or gastric injury are (or were) present, urgent endoscopy is recommended to exclude esophageal injury.
- Consult with Gastroenterology if > 1 battery ingested to discuss possible removal.
- Allow batteries to pass spontaneously if they have passed beyond the esophagus (stomach and beyond) and no clinical indication of significant gastrointestinal injury is evident. Manage the patient at home on a regular diet. Encourage activity. Avoid unnecessary endoscopic or surgical removal in asymptomatic patients. Promptly re-evaluate all patients who develop signs or symptoms possibly related to the battery. Endoscopic removal of batteries still in the stomach should be pursued for even minor symptoms. For batteries beyond the reach of the endoscope, surgical battery removal may be required in the unusual patients with evidence of occult or visible bleeding, abdominal pain, profoundly decreased appetite, vomiting, signs of an acute abdomen, and/or fever, unless these clinical manifestations are clearly unrelated to the battery. Confirm battery passage by inspecting stools. Consider repeat radiographs to confirm passage if passage not observed in 48 hours. Repeat serial radiographs thereafter (in 7-10 days) until passage confirmed. Confirming passage may avoid urgent diagnostic intervention for minor symptoms developing later.
- Manage ingestion of a hearing aid containing a battery as an ingestion of a small battery (≤ 12 mm).
- Avoid these ineffective, unnecessary or unproven therapeutic interventions:
- Ipecac administration (ineffective).
- Blind battery removal with a balloon catheter or a magnet affixed to a nasogastric tube (can’t determine extent of injury).
- Blood or urine concentrations of mercury, lithium, or other battery ingredients (unnecessary).
- Chelation (unnecessary).
- Laxatives (ineffective) or polyethylene glycol electrolyte solution (unproven effectiveness and unknown if solution enhances electrolysis). Charcoal (no role).
References:
Litovitz T, Whitaker N, Clark L, White NC, Marsolek M. Emerging battery ingestion hazard: Clinical implications. Pediatrics 2010;125(6):1168-1177.
Kramer RE, Lerner DG, Lin T, et al. Management of ingested foreign bodies in children: a clinical report of the NASPGHAN Endoscopy Committee. J Pediatr Gastroenterol Nutr. 2015; 60(4):562–74.
Leinwand K, Brumbaugh DE, Kramer RE. Button battery ingestion in children: a paradigm for management of severe pediatric foreign body ingestions. Gastrointestinal Endoscopy Clinics of North America 2016;26(1):99-108.
Jatana KR, Rhoades K, Milkovich S, Jacobs IN. Basic mechanism of button battery ingestion injuries and novel mitigation strategies after diagnosis and removal. Laryngoscope 2017; 127(6):1276-1282.
Anfang RR, Jatana KR, Linn RL, Roades K, Fry J, Jacobs IN: pH-neutralizing esophageal irrigations as a novel mitigation strategy for button battery injury. Laryngoscope 2018 Jun 11; Epub ahead of print.


